But what if there were a better way?
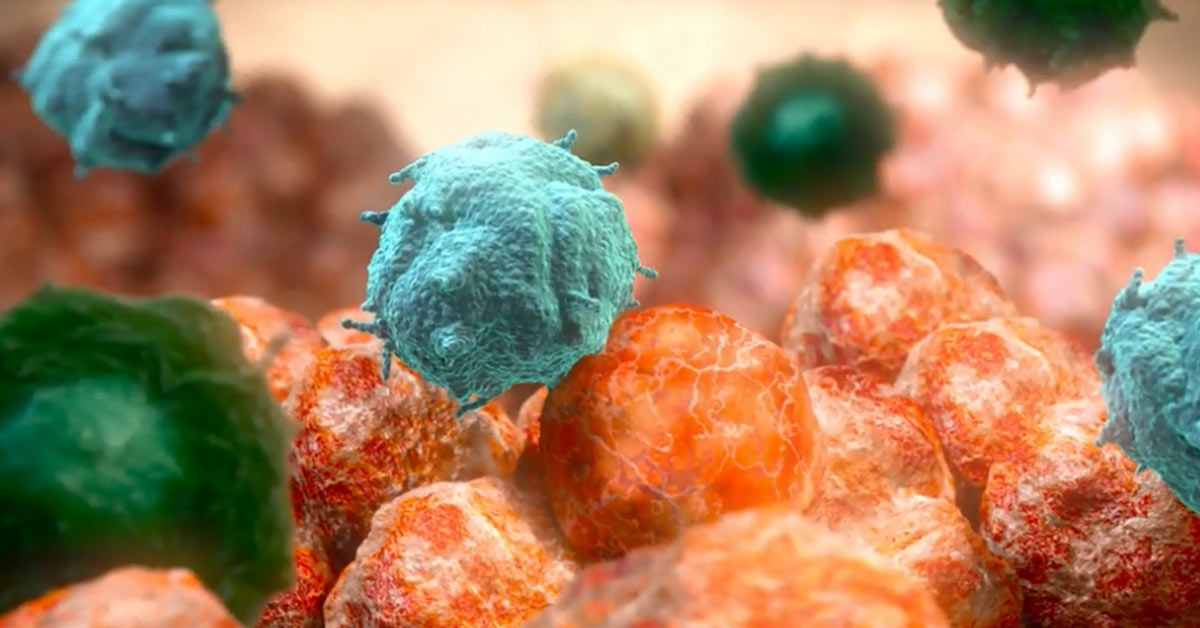
By studying the interactions between a tumor and a patient’s immune system, researchers at biopharmaceutical companies such as Bristol-Myers Squibb (BMS) are trying to reduce the ambiguity involved in fighting cancer. In a healthy person, the immune system detects a cancerous or mutated cell and activates cytotoxic T cells, which recognize the tumor cell and target it for elimination. This process happens naturally in the body multiple times per day. But some tumor cells have mechanisms to evade or suppress the immune response, allowing them to grow without restraint.
BMS researchers are trying to understand these immune-evasive mechanisms, in the hope that they can block them, and allow the body to eliminate the cancer on its own. This topic was recently discussed in Scientific American.
For instance, human cells have what’s called “immune checkpoint receptors,” which put the brakes on the immune system and prevent it from attacking healthy cells. One of these receptors, known as PD-1 (programmed death-1), alerts the T cells to suppress the immune response, which prevents the body from attacking itself in a healthy person. However, some tumors are able to stimulate the production of PD-1, causing the T cells to become exhausted and lose their ability to fight the cancer.
Not every cancer cell works this way, however, meaning that treatment that inhibits a tumor’s ability to rely on checkpoint receptors will only work in some patients. Researchers are trying to locate the biomarkers in cancer cells, so they can determine the most effective treatment.